REQUIREMENTS AND RESPONSIBILITIES
Reminder: You must complete our 15-minute, CMS-required D-SNP Model of Care training
Providers play an integral role in the care teams that support our dual-eligible special needs (D-SNP) members. That's why the Centers for Medicare and Medicaid Services (CMS) requires us to make sure providers who are contracted with us to see PriorityMedicare patients are trained on our Model of Care.
Our Model of Care is a quality improvement tool that ensures the unique needs of our D-SNP members are met and describes the processes and systems we use to coordinate their care.
Who needs to complete Model of Care training?
- All providers who are part of the Priority Health Medicare Advantage network
- Out-of-network providers who see at least five D-SNP members
This includes specialists, ancillary providers and anyone part of an ICT (interdisciplinary care team) for a D-SNP member. This is a CMS requirement.
Your Provider Strategy & Solutions Consultant will reach out to you with a report of providers who need to complete training and/or a report of providers who entered an incorrect NPI and need to re-attest to training.
How to access training
You can choose to group our training with any existing, required training (like compliance training) or use our 15-minute on-demand webinar.
Refer to our Provider Manual for details on how to complete training.
Training needs to be completed and attested to by Dec. 31, 2024. Late submissions will not be accepted.
BILLING AND PAYMENT
Starting Dec. 9, submit new or corrected claims when you get a retroactive authorization after a claim denial
There will soon be a new requirement for claims processing when a retroactive authorization has been granted after a claim denial.
What’s changing?
Starting Dec. 9, 2024, we’ll require you to submit a claim for payment if a retroactive authorization is approved after a claim has denied (fully or partially) for no authorization:
- Claim denied in full → submit a new claim
- Claim partially denied → submit a corrected claim with the authorization number listed in the notes section
What’s not changing?
Our medical authorization appeals process isn’t changing. If you appeal a denied authorization request and we grant a retroactive authorization during this appeals process, there’s no need to submit a new claim if a claim had previously been denied. Our teams will continue to reprocess these denied claims for payment automatically.
Void claims now appear on remittance advice with original claims
In June 2024, we changed how we process your void claims (claims submitted to cancel a previous claim) to align with industry standards, for both UB-04 and HCFA-1500 claim forms.
Previously, we would close the void claim, and you would see just one claim adjustment on your remittance advice (RA) for the original claim’s payment recovery. Now, you’ll see adjustments for both the void claim and original claim as follows:
RA type
Adjustment codes you’ll see
Paper RA
Void claim (denial): K49 – Claim has been cancelled or voided
Original claim (payment recovery): OX6 – Charge billed in error
Electronic RA (835)
Void claim (denial): CARC 18 – Exact duplicate claim/service
Original claim (payment recovery): CARC 16 (Claim/service lacks information or has submission/billing error(s)) and RARC M79 (Missing/incomplete/invalid charge)
Please note, we won’t process appeals on void claim denials.
Reminder: Informal claim reviews are required before appeals
It’s important to us that we accurately process your claims, and you understand the way your claims are handled.
To support you through the claim dispute process to make sure your questions / concerns are addressed in a timely manner – and you’re paid accurately and fairly for the care you’ve provided to our members – we’re sharing a few reminders and tips for our claim review and appeal process.
Understand how your claim processed
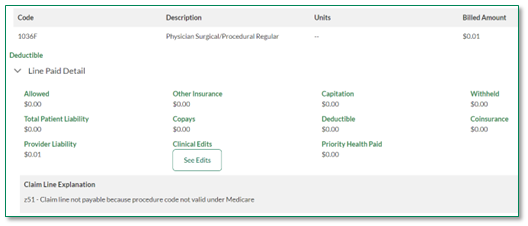
In prism, you can see exactly how a claim processed and, if it was denied, why. To do this:
- Log into your prism account.
- Under the Claims menu, click Medical Claims.
- Search for and click the Claim ID in question.
- Scroll down to see line paid details, including any denial explanation. If a clinical edit applied to the claim, a See Edits button will appear, which takes you to an explanation of the edit(s).
If you’re unable to find the information you need in prism, you can reach out to our teams for help. Learn how.
Follow our two-step claim dispute process
The claim dispute process includes two steps:
- Informal claim review – This step, including a review decision from our team, is required before an appeal can be processed. You must wait 45 days after submitting a claim, to allow claim processing, before submitting a claim review asking us to reconsider our decision on a claim. This may include a comprehensive review, coding / clinical edit questions, third party liability, coordination of benefits and more.
- Claim appeal – If you’re unsatisfied with the outcome of the claim review, you can submit an appeal. Appeals can dispute payment issues, clinical edits and claim denials. Please note, you have one appeal right per claim. Any future claim corrections won’t result in additional appeal rights.
Review tips & tricks
We recently updated our claim reviews and appeals tipsheet to include even more helpful information, including answers to common questions like:
- What’s the different between a claim review and appeal, and when can you use them?
- What makes a good appeal?
- What sort of documentation can you submit with an appeal?
- What about reviews for multiple claims?
- And more
Please consider sharing this tipsheet with your teams that handle billing and appeals.
PLANS AND BENEFITS
Southwest Michigan providers: Medicaid rebid changes do NOT impact Medicare
Changes impacting Priority Health Medicaid members resulting from the recent Medicaid rebid do not impact member eligibility for any other plan types, including Marketplace, Medicare, MAPD, D-SNP or Medigap plans.
The rebid also does not impact your Priority Health network participation—it only changes the regions in which members can sign up with Priority Health Medicaid.
Southwest Michigan providers: Do not turn away any Priority Health members based on their plan type. Please continue to see new and existing Priority Health patients with any plan you participate with, checking their eligibility before you see them just as you did before.
How do I check patient eligibility?
To confirm that a patient is a current Priority Health plan member, use the Member Inquiry tool on prism. If you don’t have a prism account, you can check eligibility by calling the Provider Helpline at 800.942.4765, option 1.
Again, the Medicaid rebid does not impact which members you can see. Continue to see any Priority Health member whose plan you are in-network for.
Does Priority Health still cover Medicaid members outside of Southwest Michigan?
Yes, Priority Health Medicaid is still in West Michigan and Metro Detroit. We also now offer Medicaid coverage in Northern Michigan (Lower Peninsula). See our service area map for exact counties.
Can Southwest Michigan providers continue to see Medicaid members from other regions?
Yes, the rebid didn’t remove providers in Southwest Michigan from our Medicaid network, it only changed the coverage of member’s who live in that region. If you are part of the Priority Health Medicaid network in any region of the state, you can continue to see Medicaid members from anywhere in Michigan.
Is Priority Health Medicare covered everywhere in the Lower Peninsula of Michigan?
Yes, Priority Health Medicare plans cover members throughout the Lower Peninsula. There are no Lower Peninsula counties where we don’t cover Medicare members, including Dual-eligible Special Needs Plan (D-SNP) members who qualify for both Medicare and Medicaid. We also cover individual MyPriority members and employer group members throughout the entire Lower Peninsula. The Medicaid rebid did not impact member eligibility for any of these plan types.
Where can I go for other questions about the Medicaid rebid?
See our provider news update about the rebid for an overview and see our provider FAQs for more details.
TRAINING OPPORTUNITIES
Register now to learn about our 2025 DBM program on Oct. 29
Join us for a webinar to learn more about the 2025 Disease Burden Management (DBM) program. This session will cover:
- Elements from the 2024 DBM program that will carry over into 2025
- What's changing in 2025, including 2 new program incentives
- How to be successful in risk adjustment and the 2025 DBM program
Can’t join us?
All webinars are recorded and posted to our website within a week of the event, so you can watch at your convenience.
INCENTIVE PROGRAMS
End of year record requests are underway
Through the end of 2024, our Risk Adjustment team will contact select providers via fax and email to request medical records to validate encounter data and hierarchical condition categories (HCC) recapture scores for the Disease Burden Management (DBM) program.
What do you need to do?
If you’re contacted by our Risk Adjustment team, please follow the instructions in the communication you receive and send all requested documentation via your preferred delivery method by Jan. 30, 2025.
Questions?
Contact your Provider Strategy and Solutions Consultant or Molly Lacy, Manager of Risk Adjustment, at molly.lacy@priorityhealth.com.
PRIORITY HEALTH
prism update: simplifying EFT setup
We’ll soon simplify our electronic funds transfer (EFT) setup process in prism, making it easier for us to work together on your EFT setup and management needs.
What’s changing?
This month, our electronic funds transfer (EFT) setup form will be moved from prism’s Resources menu to the General Requests section. The form fields and information requested will remain the same but will look a little different.
The current EFT setup form takes you outside of prism to complete your request, and we communicate with you via email.
With this update, all EFT setup requests will create a prism inquiry, allowing you to submit, track and receive our updates on your requests directly in prism. No separate form or emails required.
How do you submit EFT setup requests?
If you’d like to receive claim payments from us by direct deposit to your bank account rather than paper check (or to change or cancel your existing EFT enrollment), follow this process:
- Log into prism.
- Click General Requests in the main menu then New Request.
- Select Register for EFT from the list of inquiry types.
- Complete all fields and click Send.
See our recent news item for screenshots of this process and what it will look like in prism.
How will you hear back?
EFT inquiries will appear in the General Requests section of prism after submission. We’ll respond within 30 calendar days. To see our response in prism, providers should go to General Requests, open the inquiry and look at the Comments section. They’ll receive an automated email notification when a comment has been entered on the inquiry.