REQUIREMENTS AND RESPONSIBILITIES
November 2024 medical policy updates
Our Medical Advisory Committee (MAC), comprised of Priority Health network physicians, met in November and approved a series of medical policy updates. Below is a summary of the updates made.
New medical policies & policies addressing updated coverage
Continuous Glucose Monitoring and Insulin Pumps (#91466)
Policy update effective Feb. 1, 2025
The following services will change from not medically necessary to medically necessary when InterQual criteria are met:
- S1034: Artificial pancreas device system (e.g., low glucose suspend [LGS] feature) including continuous glucose monitor, blood glucose device, insulin pump and computer algorithm that communicates with all of the devices
- S1035: Sensor; invasive (e.g., subcutaneous), disposable, for use with artificial pancreas device system
- S1036: Transmitter; external, for use with artificial pancreas device system
- S1037: Receiver (monitor); external, for use with artificial pancreas device system
Applicable InterQual criteria are available in CP: Durable Medical Equipment under Continuous Glucose Monitors, Insulin Pumps, and Automated Insulin Delivery Technology.
Digital Therapeutics (#91645)
Policy effective Dec. 1, 2024
This new policy addresses a new area of technology, digital therapeutics (DTx), that’s becoming more prevalent and puts current Priority Health policy and system configuration into writing for transparency.
DTx are health software intended to treat or alleviate a disease, disorder, condition or injury by generating and delivering a therapeutic medical intervention. DTx, including the DTx software and any associated ancillary components, aren't medically necessary for any indication or use, and are experimental, investigational or unproven due to insufficient evidence in current published peer-reviewed literature to support clinical utility and efficacy.
This policy addresses only digital therapeutics. The criteria are not applicable to the medical, behavioral health or pharmacological therapies/treatments or medical devices used in conjunction with digital therapeutics.
Renal Denervation for Resistant Hypertension (#91644)
Policy effective Feb. 1, 2025
This new policy provides medical necessity criteria for the ablation of the renal sympathetic nerves using radiofrequency or ultrasound for the treatment of resistant hypertension. Within the scope of this policy, CPT codes 0338T and 0339T are covered for:
- Medicare effective Oct. 1, 2024
- Commercial effective Feb. 1, 2025, with prior authorization
Retired medical policies
Effective Dec. 1, 2024
- Computerized Tomographic Angiography - Coronary Arteries (CCTA) (#91614)) – This policy didn’t include Priority Health medical criteria, instead referring to EviCore for management / medical necessity determination through EviCore’s relevant guidelines. Providers should refer to EviCore’s guidelines.
- Transcutaneous Electrical Acustimulation (TEAS) For Hyperemesis Gravidarum (#91576)– This policy had a narrow scope that didn’t require it to be a standalone policy. The language it contained has been added to the Peripheral Nerve Stimulation policy (#91634).
Additional medical policy updates
Effective Dec. 1, 2024
The following policies were updated to clarify language or to align with updated industry standards. See the policy changes list in our Provider Manual for details on each policy update.
- Electrophysiology Testing & Catheter Ablation for Cardiac Arrhythmias (#91314)
- Feeding Disorders (#91469)
- Gender Affirming Surgery (#91612)
- Gender Dysphoria Non-Surgical Treatment (#91622)
- Implantable Heart Failure Monitors (#91610)
- Infusion Services & Equipment (#91414)
- Orthognathic Surgery (#91273)
- Peripheral Nerve Stimulation (#91634)
- Platelet Rich Plasma/Platelet Rich Fibrin Matrix/Autologous Blood-Derived Products/BMAC (#91553)
- Pulse Oximetry for Home Use (#91452)
- Septoplasty/Rhinoplasty (#91506)
- Surgical Treatment of Obesity (#91595)
- Vision Care (#91538)
Reminder: You must complete our 15-minute, CMS-required D-SNP Model of Care training
Providers play an integral role in the care teams that support our dual-eligible special needs (D-SNP) members. That's why the Centers for Medicare and Medicaid Services (CMS) requires us to make sure providers who are contracted with us to see PriorityMedicare patients are trained on our Model of Care.
Our Model of Care is a quality improvement tool that ensures the unique needs of our D-SNP members are met and describes the processes and systems we use to coordinate their care.
Who needs to complete Model of Care training?
- All providers who are part of the Priority Health Medicare Advantage network. (All providers aligned with this network must complete the MOC training, regardless of whether they participate in Medicaid.)
- Out-of-network providers who see at least five D-SNP members
This includes specialists, ancillary providers and anyone part of an ICT (interdisciplinary care team) for a D-SNP member. This is a CMS requirement.
Your Provider Strategy & Solutions Consultant will reach out to you with a report of providers who need to complete training and/or a report of providers who entered an incorrect NPI and need to re-attest to training.
How to access training
You can choose to group our training with any existing, required training (like compliance training) or use our 15-minute on-demand webinar.
Refer to our Provider Manual for details on how to complete training.
Training needs to be completed and attested to by Dec. 31, 2024. Late submissions will not be accepted.
BILLING AND PAYMENT
New and updated billing policies are available in our Provider Manual
We’ve posted several new and updated billing policies, which align to industry standards, to the Provider Manual.
Policies going into effect Jan. 20, 2025
The following policies and policy updates will go into effect on Jan. 20, 2025. Below are links and a high-level overview of each policy. Please see each policy for specific billing, coding and reimbursement details.
- Prosthetic orthotics and footwear: This new policy sets billing and coding standards – in alignment Centers for Medicare and Medicaid Services (CMS) local coverage determinations (LCDs) and local coverage articles (LCAs) – for orthopedic footwear, ankle-foot orthosis (AFO) and knee-ankle-foot orthosis (KAFO).
- Fundus photography: Using a retinal camera to photograph regions of the vitreous, retina, choroid and optic nerve – fundus photography documents abnormalities of disease processes affecting the eye or follows the progression of a disease. In alignment with HEDIS and CMS LCDs and LCAs, this new policy identifies how this service will be reimbursed (generally no more than two times per year) and for which specific conditions.
Additional policies, new and updated
Additionally, the following policies were recently posted to or updated in the billing / coding policies page in our Provider Manual. They put our current policies and requirements into writing for transparency. Please see the individual policies for details:
- Behavioral health
- Condition codes
- Continuous Glucose Monitor (CGM) supplies
- Facility modifiers
- General coding
- Miscellaneous durable medical equipment (DME)
- Ophthalmology and vision
- Pelvic and transvaginal ultrasounds
- Portable radiology services
AUTHORIZATIONS
Peer-to-peer policy update cancelled
In June, we announced an update to our peer-to-peer (P2P) policy, which would only allow the clinical information submitted with the initial authorization request to be considered at the P2P.
After careful consideration, including assessment of feedback from our provider network, we’ve decided not to move ahead with this change, for both inpatient and outpatient authorizations.
We encourage you to continue to be thorough with your authorization requests, ensuring all supporting documentation is available and submitted with the initial request. This helps us get you the best decision the first time and helps you avoid potential re-work and appeals.
See our P2P policy for request timelines, how to request a P2P and more.
Scheduled maintenance dates and times for TurningPoint’s authorization portal
TurningPoint’s authorizations portal is intermittently offline for scheduled maintenance one evening per month, from 7 p.m. on a Saturday to 12 a.m. the following Sunday (Eastern Time).
Upcoming scheduled maintenance dates
- Dec. 7, 2024
- Jan. 11, 2025
- Feb. 15, 2025
- Mar. 15, 2025
- Apr. 12, 2025
- May 17, 2025
- June 7, 2025
- July 12, 2025
- Aug. 10, 2025
- Sept. 13, 2025
- Oct. 11, 2025
- Nov. 15, 2025
- Dec. 14, 2025
On these dates, the TurningPoint authorizations portal will be unavailable to submit authorization requests for 5–10-minute intervals between 7 p.m. to 12 a.m.
What you need to know
You may wait to submit their authorization requests until the portal is back online, or you may choose to submit via phone or fax.
- Phone: Call 313.221.5553 or 855.511.0840 (toll free)
- Fax: Submit TurningPoint’s authorization intake form to 313.261.7199 or 833.374.0036 (toll free)
PHARMACY
Express Scripts is no longer accepting new start GLP-1 prescriptions effective Dec. 1, 2024
Express Scripts, our pharmacy benefit manager, has informed us they’ll no longer accept prescriptions for new start GLP-1 medications beginning Dec. 1, 2024. After December 1, providers who submit new GLP-1 prescriptions to Express Scripts, or submit prescriptions for patients who haven’t filled a GLP-1 medication through Express Scripts in the last 180 days, will be contacted by Express Scripts and directed to an in-network retail pharmacy.
How will this impact you?
You’ll need to send GLP-1 prescriptions for your patients starting therapy to an in-network retail pharmacy, rather than Express Scripts.
What can you do to help combat ongoing GLP-1 supply shortages for your patients?
- Less than 32% of patients remain on therapy within a year of starting a GLP-1. It’s important that patients understand the potential side effects of GLP-1s and the benefits of combining this therapy with diet and exercise changes.
- If applicable, consider other classes of weight loss medications for your patients.
- Learn more with our provider handout for combatting GLP-1 shortages.
PLANS AND BENEFITS
Narrow vs. tiered networks
We’ve heard about some confusion between our narrow networks and our tiered networks, especially those with similar names, so we want to illustrate the difference using the example of the Southeast Michigan Partners tiered network and a narrow network, the Southeast Michigan Network. These are two different networks attached to different plans. They do not share the same providers, and they are not available to members in all the same counties.
What is Southeast Michigan Partners?
Southeast Michigan Partners is one of our tiered networks. It is available to employer groups through multiple HMO and POS plans in six counties:
- Livingston
- Macomb
- Oakland
- St. Clair
- Washtenaw
- Wayne
It includes multiple health systems in Tier 1:
- Ascension
- Corewell Health - East
- Detroit Medical Center
- Lake Huron Medical Center
- Michigan Medicine
- Trinity Health
Members will benefit from lower coinsurance, copays and deductibles when receiving care through a Tier 1 provider. Members still have access to the entire Priority Health network, but care received from Tier 2 providers has greater member cost sharing.
What is the Southeast Michigan Network?
The Southeast Michigan Network is one of our narrow networks. It’s a MyPrioritySM HMO narrow network plan available to individuals under 65 and their families in three counties:
- Macomb
- Oakland
- Wayne
It includes two health systems:
- Corewell Health - East
- Trinity Health
Members are only covered when receiving care from in-network providers, except in emergencies.
How can you tell which network a Priority Health member is part of?
If you’re confused about whether a patient is covered on the Southeast Michigan Partners tiered network or the Southeast Michigan narrow network, check one of two places:
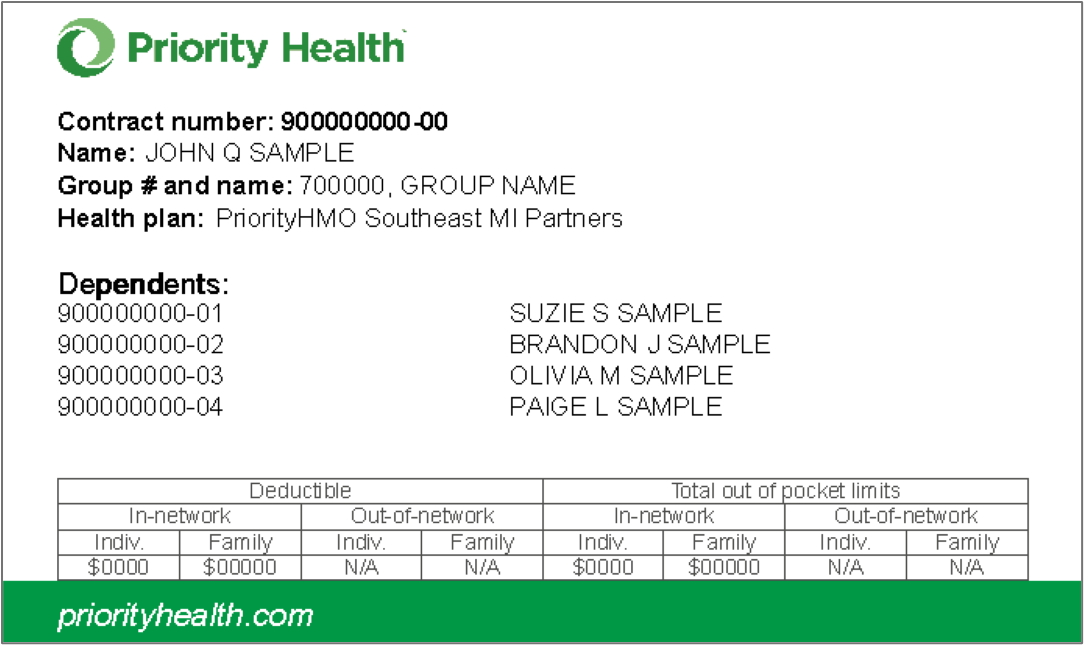
- The patient’s Priority Health member ID card.
Note the different details listed in the Health plan field on each card.
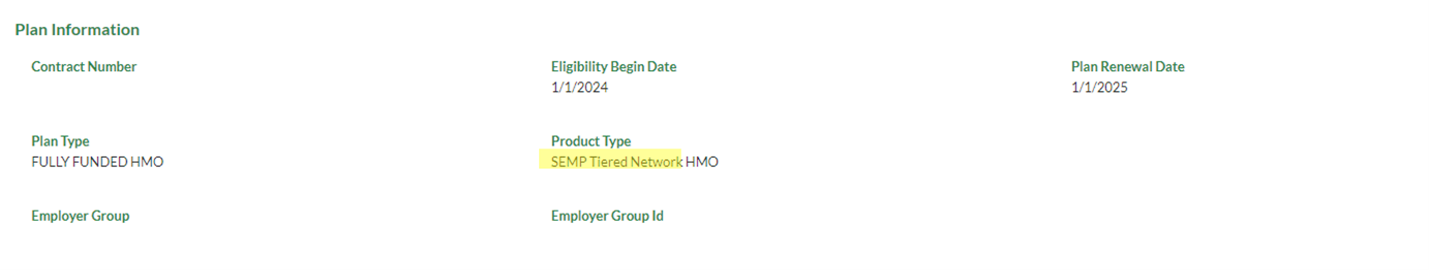
- Member Inquiry in prism. In a member’s plan information, check the “product type” listed. For members on a Southeast Michigan narrow network plan, it will say “Southeast Michigan Network.” For members on the Southeast Michigan Partners tiered network, it will say “SEMP Tiered Network,” as in the screenshot below.
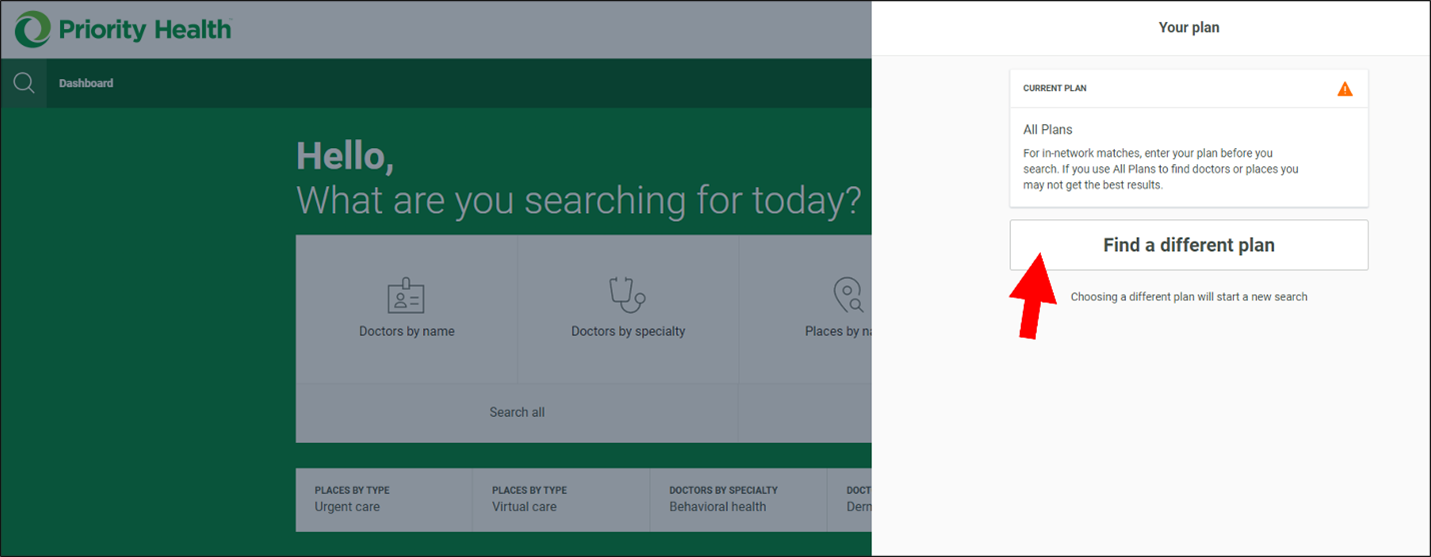
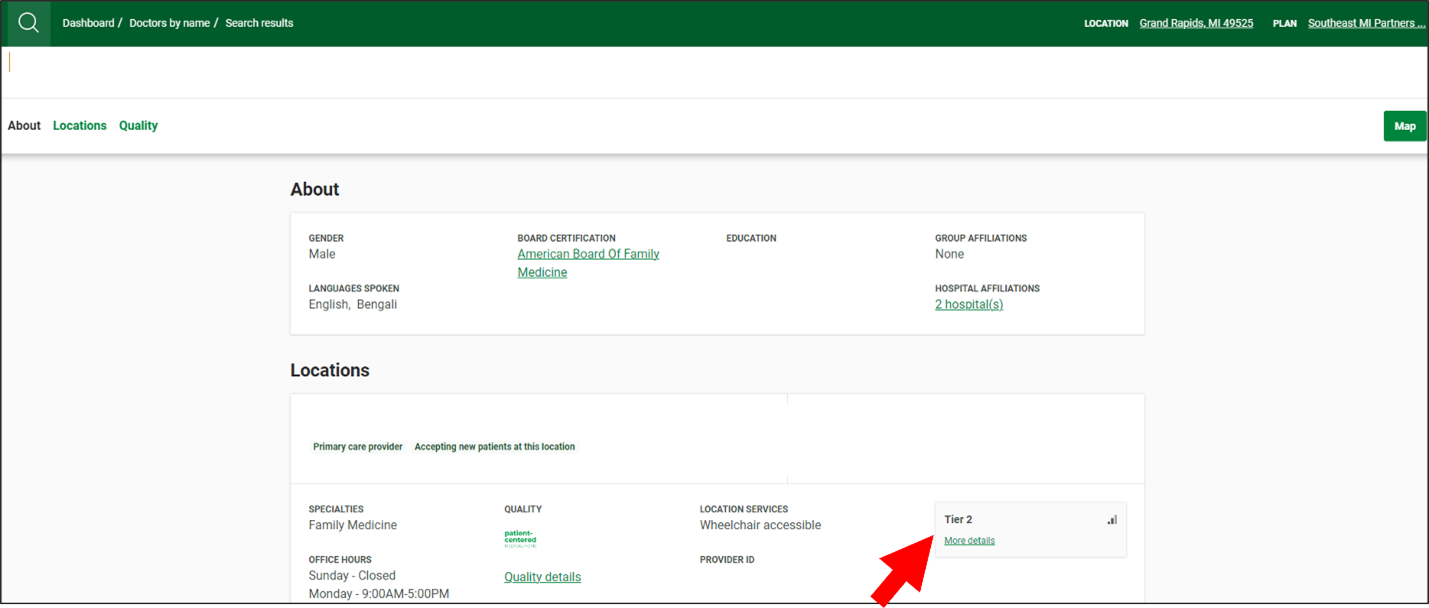
How can you tell if you or another provider is in-network?
Once you know the kind of plan your patient has, you can use our Find a Doctor tool to find in-network providers. Note that you can use Find a Doc to determine if you are in the patient’s network too.
- Search by plan type by clicking the yellow button in the upper right corner.
- Click the “Find a different plan” button.
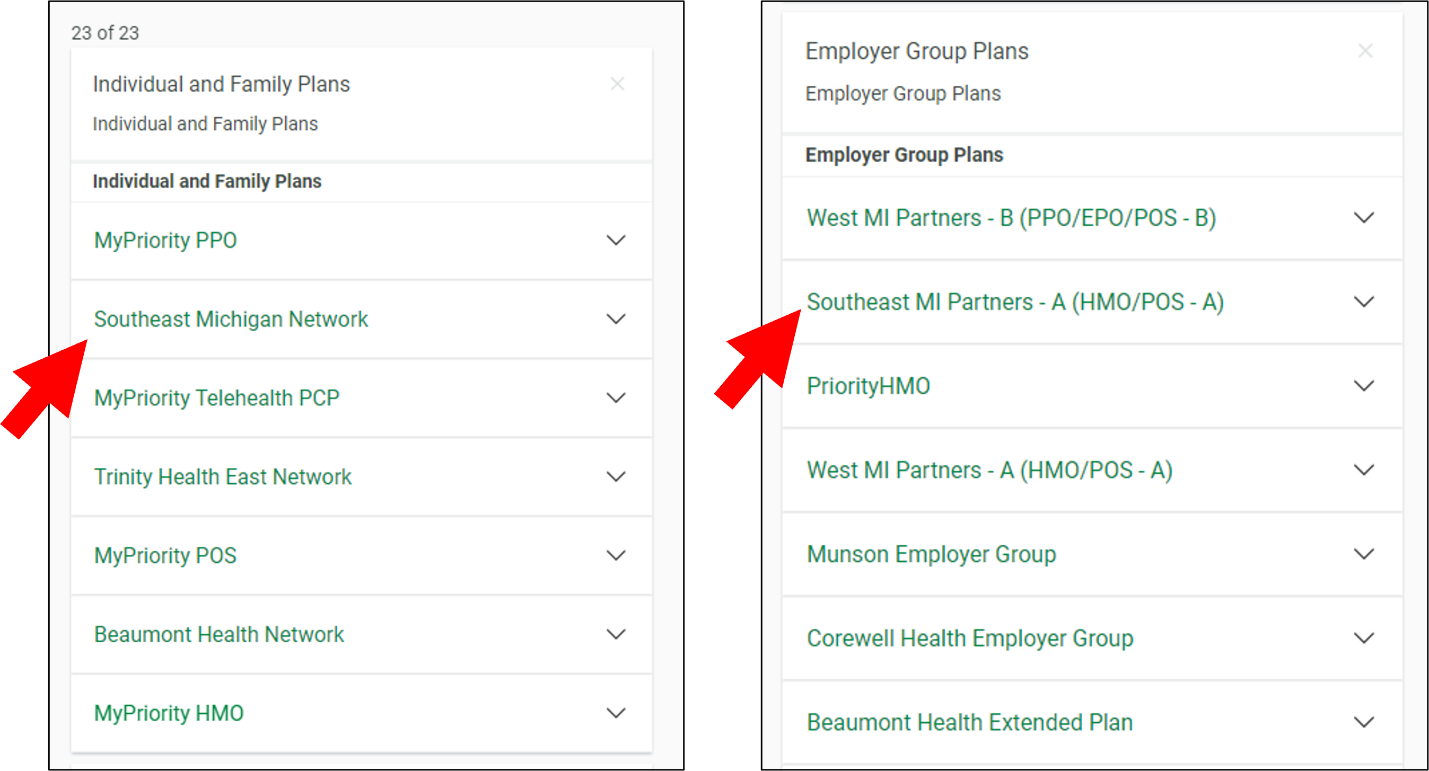
- Search “Southeast Michigan Network” for the narrow network or “Southeast MI Partners” for the tiered network. Note that there are two options for “Southeast MI Partners.” Choose option A for HMO plans or POS A plans, and option B for PPO, EPO or POS B plans. (If you’re not sure whether a plan is POS A or POS B, the “Health plan” field of the member ID card will indicate either “PriorityPOS-A Southeast MI Partners” or “PriorityPOS-B Southeast MI Partners.”)
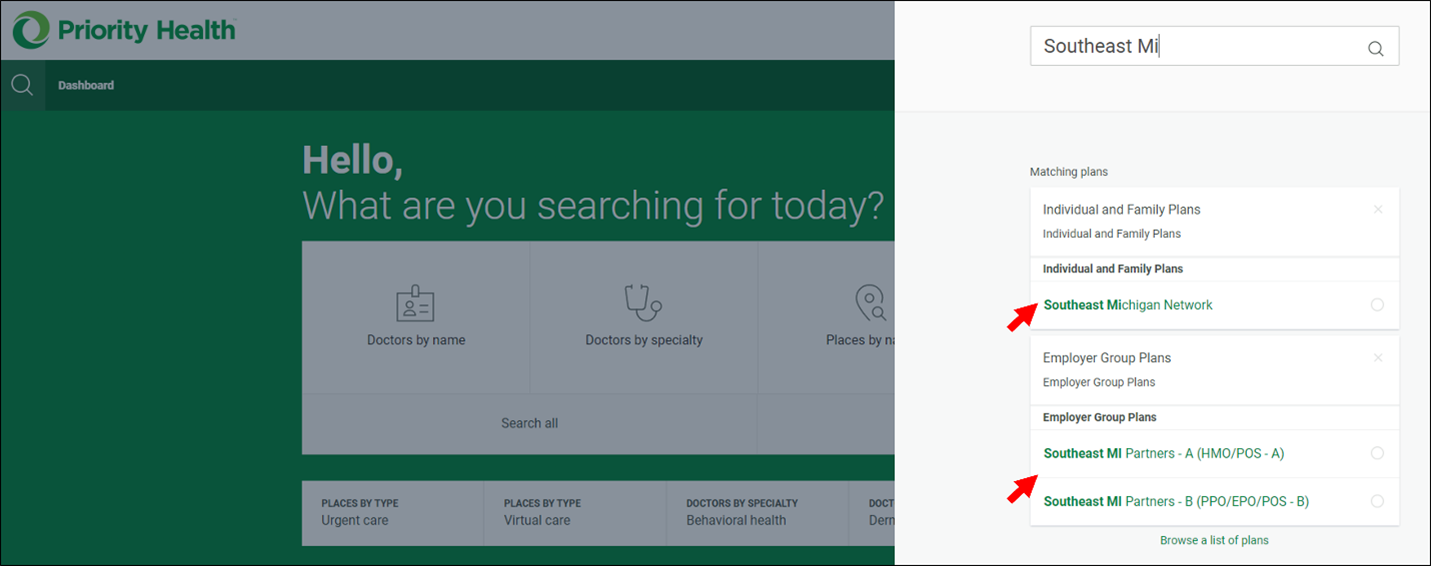
- You'll then see only in-network providers when you search. If a provider you search for is Tier 2 for a member in a tiered-network plan, the provider’s information box will tell you.
You can also search for providers in Find a Doctor without having a plan selected.
- Search for and then click the provider you want.

- Click the link in their information box under the “plans accepted” heading to bring up a list of the types of plans they accept.
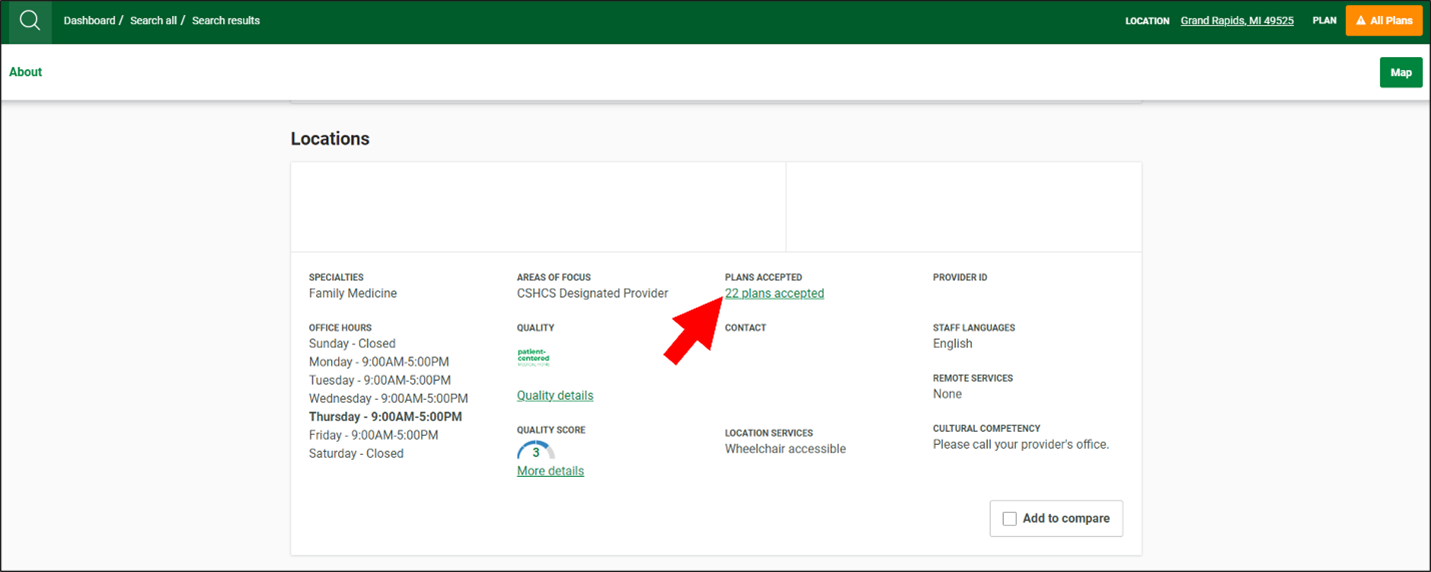
- The Southeast Michigan Network will be listed under “Individual and Family Plans” if it is an accepted plan type, and “Southeast MI Partners” will be listed under “Employer Group Plans.”
What should you do to make sure members receive in-network care whenever possible?
If you’re not sure if you're in network for a member, you can use our Find a Doctor tool by looking up the member's specific plan and seeing if they're in network. When a patient needs to be referred to another provider, providers can use Find a Doctor to find in-network care.
Need to know more about the differences between narrow and tiered networks?
Check out this helpful one-pager on narrow vs. tiered networks.
Southwest Michigan providers: Medicaid rebid changes do NOT impact Medicare
Changes impacting Priority Health Medicaid members resulting from the recent Medicaid rebid do not impact member eligibility for any other plan types, including Marketplace, Medicare, MAPD, D-SNP or Medigap plans.
The rebid also does not impact your Priority Health network participation—it only changes the regions in which members can sign up with Priority Health Medicaid.
Southwest Michigan providers: Do not turn away any Priority Health members based on their plan type. Please continue to see new and existing Priority Health patients with any plan you participate with, checking their eligibility before you see them just as you did before.
How do I check patient eligibility?
To confirm that a patient is a current Priority Health plan member, use the Member Inquiry tool on prism. If you don’t have a prism account, you can check eligibility by calling the Provider Helpline at 800.942.4765, option 1.
Again, the Medicaid rebid does not impact which members you can see. Continue to see any Priority Health member whose plan you are in-network for.
Does Priority Health still cover Medicaid members outside of Southwest Michigan?
Yes, Priority Health Medicaid is still in West Michigan and Metro Detroit. We also now offer Medicaid coverage in Northern Michigan (Lower Peninsula). See our service area map for exact counties.
Can Southwest Michigan providers continue to see Medicaid members from other regions?
Yes, the rebid didn’t remove providers in Southwest Michigan from our Medicaid network, it only changed the coverage of member’s who live in that region. If you are part of the Priority Health Medicaid network in any region of the state, you can continue to see Medicaid members from anywhere in Michigan.
Is Priority Health Medicare covered everywhere in the Lower Peninsula of Michigan?
Yes, Priority Health Medicare plans cover members throughout the Lower Peninsula. There are no Lower Peninsula counties where we don’t cover Medicare members, including Dual-eligible Special Needs Plan (D-SNP) members who qualify for both Medicare and Medicaid. We also cover individual MyPriority members and employer group members throughout the entire Lower Peninsula. The Medicaid rebid did not impact member eligibility for any of these plan types.
Where can I go for other questions about the Medicaid rebid?
See our provider news update about the rebid for an overview and see our provider FAQs for more details.