PriorityActions issue for May 23, 2024 highlights:
INCENTIVE PROGRAMS
ACNs must organize providers into practice groups in PRA by October 15
The 2025 PCP Incentive Program (PIP) will be run at the practice level, including reporting and settlement. To make this possible, we must have accurate, consistent practice group data in our Provider Roster App (PRA) tool for each ACN.
By the November 2024 attestation cycle, which runs from October 1-15, all ACNs must have their providers organized into practices using PRA’s Group / Subgroup feature.
Your Provider Strategy & Solutions Consultant will follow-up with you via email to share your current PRA practice group organization status and discuss any necessary next steps.
Updated 2024 HEDIS Provider Reference Guide available
We recently updated our 2024 HEDIS Provider Reference Guide (login required).
To access the guide, log into your prism account and navigate to Provider Incentive Programs, then Quality Improvement. You can then bookmark the manual URL in your browser for quick access.
Here’s a summary of the changes:
Glycemic Status Assessment for Patients with Diabetes (GSD) measure
Updated verbiage to state that Medicare patients are considered controlled if A1c is < 9.0%.
Kidney Health Evaluation for Patients with Diabetes (KED) measure
Updated numerator compliance to include:
- At least one eGFR
- At least one uACR identified by either of the following:
- A uACR or
- Both a quantitative urine albumin test and a urine creatinine test with service dates four days or less apart. For example, if the service date for the quantitative urine albumin test was December 1 of the measurement year, then the urine creatinine test must have a service date on or between November 27 and December 5 of the measurement year.
Billing codes were updated for the following measures:
- Prenatal and Postpartum Care (PPC)
- Chlamydia Screening in Women (CHL)
- Eye Exam for Patients with Diabetes (EED)
- Care for Older Adults (COA) – Functional Status Assessment
- Care for Older Adults (COA) – Medication Review
- Care for Older Adults (COA) – Pain Assessment
- Advance Care Planning (ACP)
- Adults’ Access to Preventive/Ambulatory Health Services (AAP)
- Lead Screening in Children (LSC)
- Child and Adolescent Well-Care Visits (WCV)
- Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (WCC)
-
Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics (APP)
Updated 2024 PIP Manual available
We recently updated our 2024 PCP Incentive Program (PIP) manual (login required).
To access the manual after logging into your account through the link provided, click PCP Incentive Program in the menu then click the Get the 2024 PIP Manual button. You can then bookmark the manual URL in your browser for quick access.
Here’s a summary of the changes:
Administrative details (pg. 9)
Under the Priority Health quality index scores definition, we clarified the description of the calculation for quality index scores (the word “plan” was missing from the last sentence in the first paragraph).
Submitting exclusions and more to our HEDIS team (pg. 11)
- Bolded the statement that submitting documentation to HEDIS email inbox for PIP care gap closure should only be used as “when all other gap closure measures have been exhausted”
- Added that the subject line of these email submissions should say “PIP Gaps in Care” to ensure timely processing
Appendix 2: Guidelines for reporting gap closure (pg. 34)
- Added information on Electronic Clinical Data Systems (ECDS)
- Added more detail to the audit findings section to align with the HEDIS Provider Reference Guide and the HEDIS ECDS Provider Guide
Appendix 5: Report inventory (pg. 41)
- Added detail on the new ACN Measure Performance (PIP_003 TAB) report
- Clarified that the PIP Gaps in Care Immunizations (PIP_011I TAB) report only includes members who are not meeting the incentivized immunization measures.
REQUIREMENT AND RESPONSIBILITIES
May 2024 medical policy updates
Our Medical Advisory Committee (MAC), comprised of network physicians contracted with Priority Health, met in May and approved the medical policy updates described below.
Unless otherwise noted, the following updates will go into effect on June 1, 2024.
New medical policy
Computer Assisted Surgical Navigation (#91641)
This policy was developed to address the surge of computer assisted surgical (CAS) navigation technologies. The policy currently only addresses CAS navigation bronchoscopy, and the medical criteria follow National Comprehensive Cancer Network non-small cell lung cancer guidelines. The policy does not change existing coverage.
Coverage change
Experimental/Investigational/ Unproven Care/Benefit Exceptions (#91117)
Effective July 1, 2024, two codes for temporary prostatic stents (C9769 and 53855) will no longer be covered for Commercial and Medicaid lines of business.
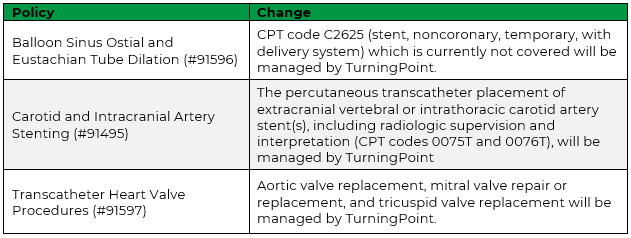
Policies impacted by the TurningPoint cardiac program
These updates will take place when the cardiac authorizations program goes live. The following medical policies will be retired because the procedures within their scope will be managed by TurningPoint Healthcare Solutions LLC (TurningPoint) through our new cardiac surgical authorizations program.
- Cardioverter Defibrillators (#91410)
- Drug Eluting Stents for Ischemic Heart Disease (#91580)
- Implantable Loop Recorder (#91618
- Percutaneous Left Atrial Appendage Closure (#91618)
- Renal Artery Stenosis (#91561)
The following medical policies will be updated to indicate specific procedures will be managed by TurningPoint.
Updated medical policies
The following policies were updated to clarify language and experimental & investigational positions, or to align with updated industry standards.
- Breast Related Procedures (#91545)
- Cellular & Gene Therapy (#91638)
- Cosmetic and Reconstructive Surgery Procedures (#91448)
- Endoscopic Submucosal Dissection (ESD) (#91617)
- Enteral Nutritional Therapy (#91278)
- Hemophilia Management (#91569)
- Markers for Digestive Disorders (#91583)
- Peroral Endoscopy Myotomy (POEM) (#91616)
- Psychological Evaluation and Management of Non-Mental Health Disorders (#91546)
- Spine Procedures (#91581)
- Stem Cell or Bone Marrow Transplant (#91066)
- Stimulation Therapy and Devices (#91468)
- Transplant of Solid Organs (#91272)
For complete descriptions of the updates made:
Action for prism Security Administrators: mandatory annual pSA renewal process begins June 1
Our annual prism Security Administrator (pSA) renewal period begins on June 1. pSAs will have until Aug. 1 to review and either approve or deny all user affiliations for your group or facility.
What exactly is happening?
Each provider group and/or facility needs a pSA to control access to data like claims, authorizations and appeals. pSAs control access by approving or denying affiliation requests. During this annual pSA renewal period, pSAs review affiliation requests they’ve already approved to make sure each user’s access is still needed.
If a user’s affiliation is renewed by their pSA, nothing will change for that user. If a user’s affiliation is denied, that user will lose access to all of that group or facility’s data.
Important: If users aren’t renewed, they'll automatically be removed from the provider affiliation after Aug. 1. It’s important for pSAs to review all renewals and take action to ensure access isn’t disrupted.
Why is this important?
Data security is a top priority in the health care industry, now more than ever. The high job turnover rate in the health care industry creates a potential vulnerability in data security. Requiring pSAs to review their affiliated users annually is a simple and quick way to safeguard provider data and protected health information (PHI) by ensuring individuals who leave their organization no longer have access to their data.
How do I complete the pSA renewal process?
If you're a pSA, follow these steps between June 1 and Aug. 1:
- In your prism account, select Security Administration, then Affiliation Requests.
- Navigate to your Affiliations table and select Affiliation Renewals at the far right of the table.
- Review the users currently affiliated with your provider group/facility and determine if they should be renewed. Once you select the user by checking the box, an Approve or Deny button will appear. Note: you can select multiple users at one time to approve or deny.
- Confirm your selection.
Unsure if the users are still employed by your organization or need to check with another department before you renew? You can select Download Pending Renewals to get an Excel sheet to share with others.
If you're not a pSA, you don’t need to do anything.
Will users be notified of the results of the review?
Users will only be notified if their renewal is denied. They’ll be sent an email and given instructions for how to submit a new request for access, in case they feel they’ve been incorrectly denied.
Don’t know if you have a pSA assigned?
- Go to your prism profile and find your list of affiliations.
- Scroll to the far right of the table and select “Show pSA details.” If you don’t have this option, a pSA hasn’t been assigned to this affiliation.
- You can contact the pSA assigned to each affiliation to confirm your access will be renewed, but it’s not required.
Questions?
Visit the prism resources page in our Provider Manual, where there are guides, FAQs and help line numbers listed.
BILLING AND PAYMENT
Reminder: Follow ICD-10 guidelines; code the highest degree of specificity
As a reminder, when billing for both professional and facility services, it’s important to code to the highest level of specificity.
At Priority Health, we use several coding and billing resources to align correct coding guidelines for accurate claims processing. This includes criteria defined by ICD-10 coding guidelines. See our General Coding Policy, available on the Billing & coding policies page in our Provider Manual, for details.
Clinical edits are controls aligned with coding guidelines or industry standard principles to flag inappropriate coding practices, inaccurate billing or duplication of services.
Why are we issuing this reminder?
On Aug. 16, 2022, we issued a notice to the provider network for a new clinical edit for ICD-10’s Excludes1 criteria, which details diagnosis codes that shouldn’t be reported together because the two codes can’t occur at the same time.
In October 2022, the edit was turned on for professional claims. On June 4, 2024, we’ll implement the edit for inpatient and outpatient facility claims as well.
What do providers need to know?
Providers can reference the ICD-10 coding manual’s Excludes Notes section for more detail and examples. Providers may also correct and resubmit denied claims with accurately coded diagnosis codes.
Reprocessing incorrectly denied CM telephone management codes, updating offline payment process
We were experiencing an issue where some care manager telephone management claims were denying when they shouldn’t. We’re modifying the claims process slightly to fix this issue and will reprocess impacted claims for payment.
Background
In August 2023, we moved these codes to an “offline” payment process, batching payments 60 days at a time by paper check. This process allows PCPs to be paid for these important services and avoids member cost share when provided under the following circumstances:
- Within 7 days of an E/M or
- Leading up to an assessment and management service / procedure within the next 24 hours
These services are paid for fully funded commercial, Medicare and Medicaid members and some self-funded commercial members based on coverage.
What’s the issue & how are we resolving it?
Providers have been appending modifier 25 to all claims for these services. In some cases, this was causing claims to deny when they shouldn’t. We’re reprocessing all impacted claims dating back to Jan. 1, 2023.
Going forward, we’ll include all CM telephone management codes for the applicable LOBs in the offline payment process, regardless of modifier use. We do ask that providers continue to append modifier 25 to claims for CM telephone management services provided on the same day as another E/M.
Will this change impact PIP?
No, this change won’t impact your ACN’s PCP Incentive Program (PIP) participation or payout. The CM telephone management codes will continue to count towards the CM measure’s two touchpoints for 2% of your ACN’s population, even if the updated billing advice isn’t followed. The codes have been counted toward the measure all along, even when denied.
For more information on the offline payment process and the applicable CPT codes, see our recently updated news item.
TRAINING OPPORTUNITIES
Our next Virtual Office Advisory (VOA) is on June 13
Join us for our next Virtual Office Advisory webinar at noon on Thursday, June 13, and learn about:
- prism: new communication tools and pSA renewal process
- Pharmacy: July 1 formulary changes, a new member discount program and other updates
- Medication adherence reports: an update
- Behavioral health: credentialing tips and virtual support with Teladoc Mental Health
- Medicare Health Outcomes Survey (HOS) and health equity