PriorityActions June 6, 2024 Issue
Please visit the Priority Health provider site for full details.
Authorizations
Inpatient peer-to-peer policy update goes into effect Sept. 4, 2024
Effective Sept. 4, 2024, and in alignment with industry standards, inpatient peer-to-peer reviews (P2P) will only consider the clinical information submitted with the initial authorization request. We will classify any additional information submitted after the initial denial as a level 1 appeal and cancel the P2P request.
As a reminder, we offer two levels of appeal for medical authorization denials.
Be thorough with inpatient authorization requests
We recognize that, when admitting a patient to the hospital, you may need multiple days to appropriately assess and document their condition and care plan. This is why we don’t require you to notify us within 24 hours if one of our members is hospitalized. Additionally, we don’t require authorization for observation stays regardless of the length of hospitalization.
By ensuring all supporting documentation is available and submitted with the initial authorization request, you can avoid potential re-work and appeals. We’re seeking to work with you, our providers, in getting you the best decision the first time.
Get more information
Review our full P2P policy for additional information, including request timelines, when P2Ps aren’t available, how to request a P2P and more.
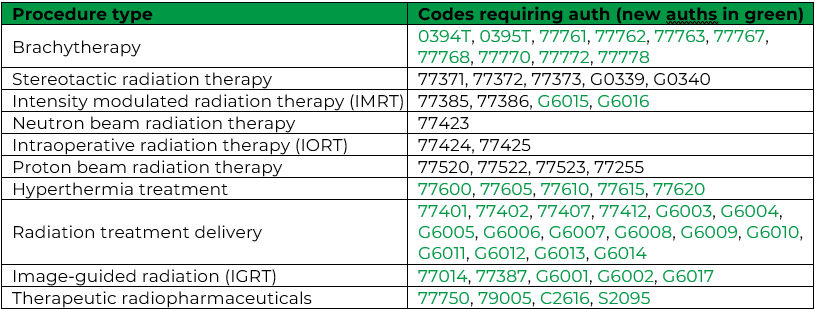
New radiation oncology authorizations program to launch this fall
We’re partnering with EviCore on a new authorization program for outpatient radiation oncology procedures. This new program is slated to launch Sept. 15, 2024.
Why work with EviCore?
The science and evidence behind radiation oncology is rapidly evolving, and the field requires sub-specialists to provide care and service to patients. With EviCore’s expertise, we’ll be able to ensure our members get the right care at the right site at the right time.
Their process is aligned with our clinical approach by reviewing requested care and using evidence-based guidelines to make care plan decisions.
How will the program work?
Providers will initiate the authorization request process in prism, as they do now. When an outpatient radiation oncology procedure requires authorization through EviCore, prism’s Request an Authorization page will automatically redirect the provider to EviCore’s online authorization portal.
What radiation oncology procedures will require authorization through EviCore?
Beginning this fall, the following services will require authorization through EviCore when done in an outpatient setting, for all lines of business:
What’s next?
In the coming weeks, you’ll receive additional information to ensure your providers have ample opportunity to be trained on using EviCore’s online authorization portal and to ask any questions they may have. Additional information will include:
- FAQs
- Peer-to-peer and appeals information
- Training webinars
- And more
Incentive Programs
2023 PIP settlement payments have been issued
2023 PCP Incentive Program (PIP) settlement payments were processed on June 4, 2024. Depending on your ACN’s preferred delivery method, checks were either processed by electronic funds transfer or postmarked to your remittance address location.
Look for an email from your Provider Strategy & Solutions Consultant with the following information:
- Indexing details for ASO/PPO
- Settlement documents, including settlement details, remittance advice and report key.
Thank you for your ongoing partnership and dedication to providing our members, your patients, high quality care.
Pharmacy
SaveOnSp ended on May 31 for select commercial members
SaveOnSP, a service that helps participating members find and enroll in manufacturer copay assistance programs for discounts on their specialty prescription drugs (Tier 4 and 5), ended on May 31 for small business commercial groups and individual members.
Why did SaveOnSP end?
Recently, the Centers for Medicare and Medicaid Services (CMS) released a new rule classifying all health plan covered drugs as essential health benefits (EHB). Prior to this, only drugs that met a specific benchmark could be considered EHB. Because SaveOnSP focused solely on securing copay assistance for non-EHB drugs, the program is no longer applicable to the impacted members.
Can members still get manufacturer copay assistance?
Yes. Manufacturer copay assistance may still be available through the drug manufacturer; however, members must enroll on their own.
How does this impact our members?
Members must either manage their own enrollment in available manufacturer assistance programs or pay the cost share for their prescriptions.
How does this impact you?
Your patients may contact you to ask about lower cost alternatives for their medications.
How are we informing members?
Impacted members will receive letters informing them of the termination of SaveOnSP and how they can use their pharmacy benefits for future prescriptions fills.
Requirements and Responsibilities
We’re contacting providers to request medical records for the Medicare Advantage Retrospective Review
We’re contacting providers to retrieve medical records for certain Priority Health members to help validate diagnoses as part of our Risk Adjustment program. If you’re contacted, please submit all requested documentation by July 9, 2024.
Why are we requesting records?
The Centers for Medicare and Medicaid Services (CMS) requires us to submit complete and accurate diagnostic data each year for each member. The data submitted is used to predict the relative health risk status of individuals during the next calendar year and must be supported by valid documentation from the medical record.
How can you submit records?
- SharePoint electronic upload:To receive a link, email RA@priorityhealth.com
- Secure email to RA@priorityhealth.com
- Fax to 616.975.8824
- Mail to
- Priority Health, Attention Risk Adjustment
1241 East Beltline Ave NE Mail Stop 2235, Grand Rapids, MI 49525
- Shipping labels are available upon request. Email your site name, package weight and list number to RA@priorityhealth.com .
- Priority Health, Attention Risk Adjustment
Remote EMR access or onsite visit: We’ve added a survey to make it easier for you to determine if your practice is eligible for remote EMR access or an onsite visit. Click below to access the survey.
Billing and Payment
Effective August 1, we’re aligning commercial DME billing and coding requirements with CMS guidelines
We’re aligning our commercial billing and coding requirements for durable medical equipment (DME) supplies to those defined by the Centers for Medicare and Medicaid Services (CMS).
The following policies – which establish reimbursable limits / frequency guidelines pulled directly from CMS local coverage determinations (LCD) and coding articles – will go into effect on Aug. 1, 2024:
Exceptions & appeals
Any exceptions to these policies will be specifically outlined in our Provider Manual or in our commercial medical policies. Providers may appeal denials for units exceeding the defined limits – appeals must be supported with medical record documentation.
Medicare & Medicaid
For Medicare claims, we’ll continue to follow CMS-defined guidelines as outlined by the Medical Affairs Committee (MAC) in national coverage determinations (NCD), LCD and Articles. Our Medicaid products will continue to follow MDHHS- and CHAMPS-defined guidelines.
See our Provider Manual’s payment policies page and continue to monitor these PriorityActions emails for additional policy alignment information.
Training Opportunities
Introducing VOA Modules and new 2024 live VOA dates
We have two announcements regarding our Virtual Office Advisory (VOA) webinars:
- We’re launching a new educational series called VOA Modules, consisting of short videos available on-demand in our online provider manual.
- We’ve scheduled additional live VOAs for the remainder of 2024, each focused on a single major topic of timely relevance.
Why are we changing the format of VOAs?
You’ve requested more targeted content for our VOAs. We’ve heard you, and we’re now offering VOA Modules and more focused live VOAs in response. Both provide precision-targeted content, so you can watch what you need without having to sit through what you don’t.
For example: rather than behavioral health providers sitting through an hour-long VOA to hear 10 minutes of content relevant to them, they can now simply go to the behavioral health category on our VOA Modules page and immediately access the content they need. Likewise, providers who need to learn about our PIP program updates can simply register for the live VOA focused solely on that, rather than waiting until the end of a multi-topic VOA.
What exactly are VOA Modules?
VOA Modules are short, on-demand versions of our VOAs. They're focused on single topics and are usually five minutes or less. They're always presented by Priority Health subject matter experts, and they’re accessed via our VOA Modules page.
What kind of content do VOA Modules cover?
You’ll find helpful tips and guides on how to work with us, including topic categories like:
- Billing and coding
- Authorizations
- Appeals
- Behavioral health
- prism
- Plans
- Disease burden management
- General
Each category has a “playlist” of Modules on topics in that category, so you can easily browse content relevant to your work.
How often are new VOA Modules added?
We’re hoping to begin at a pace of about three per month.
How will providers know about new Modules?
The VOA Modules page includes a playlist of new Modules at the top, so you can quickly see all recently posted videos. Be sure to bookmark the page so you can check back frequently.
To actively notify you, we'll send a prism notification every time new Modules drop. We'll also send out a monthly VOA roundup via PriorityActions and our provider news page to tell you about all recently posted Modules and any upcoming live VOAs.
Will all VOA features work with Modules?
Yes—although they will function differently:
- You can access links to resources via “cards” that pop up at appropriate points in the Module. (If you can’t see them, try going into full-screen viewing mode.)
- A card at the end of each Module will link you to a VOA Module survey, where you can provide feedback and future topic requests.
- At the end of all new Modules, you’ll have the option to fill out a form with any related questions you might have. We’ll respond via email.
An intro video at the top of the VOA Modules page walks you through these features.
What will live VOAs look like going forward?
For live VOAs, we're moving away from the bundled multi-topic format to single topics. Live VOAs will mainly only be used to cover topics of timely relevance, such as product and formulary changes coming on January 1st of each year.
What’s the schedule for live VOAs for the rest of 2024?
Here’s what we have on the calendar:
- July 11: 2025 PIP program overview
- Oct. 17: 2025 product updates
- Oct. 29: Disease burden management program updates
- Nov. 7: Medicare & Medicaid quality updates
- Nov. 21: January 1 formulary changes
You’ll be sent separate invites for each of these events.
Note that we may schedule additional VOAs, as needed.
Where can I find all this if I forget?
All this can be found on the VOA page in our Provider Manual, which also includes a link to our VOA Modules page.