Priority Health - PriorityActions for providers update July 11, 2024:
PHARMACY
Resource to address GLP-1 shortages and support patient medication adherence
Due to shortages of glucagon-like peptide 1 (GLP-1) drugs, we anticipate your patients—our members—may not be able to access these drugs consistently, putting them at risk of not getting the care they need. To help optimize the health outcomes of your patients and to ensure you’re meeting your diabetes medication adherence goals, our Pharmacy team put together a provider handout with considerations for prescribing GLP-1s.
Find out how you can help combat GLP-1 shortages and optimize the outcomes of patients being treated with a GLP-1.
TRAINING OPPORTUNITIES
July VOA roundup: watch new Modules and register for upcoming webinars
We have new Virtual Office Advisory (VOA) Modules, quick and informative videos, available for you and your practice to view on the following topics:
- News and updates: using online resources and tools to stay in the loop
- prism inquiries: inquiry timelines and how to get your questions resolved as quickly as possible
- Pre-service organization determinations: how to request PSODs for Medicare members and how to bill if a Medicare member proceeds with a non-covered service
- Coding tips: virtual care billing, using Edits Checker, front-end rejections and sending us questions about clinical edits
View these and more at our VOA Modules page.
Upcoming webinars open for registration
Here’s what we have on the calendar:
- July 11: 2025 PIP program overview
- Oct. 17: 2025 product updates
- Oct. 29: Disease burden management program updates
- Nov. 7: Medicare & Medicaid quality updates
- Nov. 21: January 1 formulary changes
Find these registration links and recordings of past VOA webinars on our website.
AUTHORIZATIONS
Provider trainings for TurningPoint authorizations programs
Join our utilization management team and TurningPoint staff to learn about the new cardiology and MSK authorization programs set to launch this September, as well as how to navigate and successfully request authorizations through TurningPoint.
Registration is now available for the following dates, with each session starting at 12 p.m. ET:
- August 14
- August 21
- August 28
- September 4
Can’t make it during the webinar’s scheduled time? A recording of the session will be sent to all registrants for on-demand viewing.
Outreach to high-volume providers
In the coming weeks, TurningPoint will reach out directly to high-volume cardiac and MSK provider offices. They’ll offer these providers the option to meet one-on-one with their provider relations and medical teams, either virtually or in person, to:
- Support training and education in the lead up to the programs’ launch
- Answer any outstanding questions
- Build a relationship for two-way communication and feedback
Peer-to-peer reviews for all authorization requests will follow new process by October 9
Effective Oct. 9, 2024, outpatient peer-to-peer reviews (P2P) will only consider the clinical information submitted with the initial authorization request. This update is in alignment with industry standards and with our updated inpatient P2P process, which goes into effect September 4.
We’ll classify any additional information submitted after the initial denial as a level 1 appeal and cancel the P2P request.
As a reminder, we offer two levels of appeal for medical authorization denials.
Get more information
Review our full P2P policy for additional information, including request timelines, when P2Ps aren’t available, how to request a P2P and more.
INCENTIVE PROGRAMS
Reminder: Attest to your providers’ PCMH designations in PRA
We’d like to remind you of the importance of attesting to your providers’ patient-centered medical home (PCMH) designation status in PRA during the 2024 PCP Incentive Program (PIP) performance year.
Why is this important?
Primary care providers (PCPs) must be practicing at a PCMH designated practice during the program year to qualify for our 2024 PIP Transformation of Care measures, including:
- Care Management
- Social Determinants of Health (SDoH) Screening
- SDoH z-code reporting
- Behavioral Health Collaborative Care (BHCC)
If you don’t report in the PRA tool that a PCP is part of a PCMH-designated practice, we’ll remove them from these measures (both numerator and denominator) at year-end settlement.
When and how to attest to PCMH designation
Report this designation to us in the PRA tool by the November attestation period, which takes place in October. We honor the following designation programs: BCBSM, NCQA, URAC and Joint Commission.
Step-by-step instructions on how to update a PCP’s PCMH designation status in PRA, including batch upload instructions, are outlined on page 11 of the 2024 PRA Manual (login required).
BILLING AND PAYMENT
Prism inquiry turnaround times and when to reach out to our team
We frequently get questions about our turnaround times for various inquiries made in prism and would like to share the following:
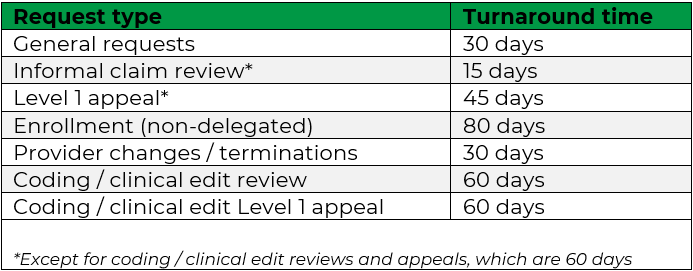
Please note the coding / clinical edit review and Level 1 appeal turnaround times have been updated to 60 days, to allow our teams sufficient time to thoroughly review the medical records and supporting documentation submitted with these inquiries.
What else do you need to know?
The turnaround times begin when the inquiry reaches the correct Priority Health team. Encourage your providers to make sure they’re selecting the most appropriate inquiry option in prism.
We ask that providers:
- Wait the full turnaround time for a response before emailing us at exceedsprocessingtime@priorityhealth.com.
- Don’t request a status update by making a comment in an open inquiry. Our system will automatically reset your turnaround timeline back to the beginning – ultimately delaying your resolution time.
- Don’t open a new inquiry to request a status update on an already open inquiry. This will cause duplicates and delay processing.