Updated TurningPoint provider training guide now available
We’ve updated the TurningPoint Provider Training Guide to include:
- Additional information requests (all plans)
- Intent to deny calls (Medicare)
- Reconsideration requests (commercial, Medicaid)
We made these updates to offer further transparency into TurningPoint’s processes, and to support you in getting the most accurate determination the first time and, if possible, avoid the appeals process.
As a reminder, TurningPoint manages cardiac and MSK authorizations on our members’ behalf.
Below is a summary of the additions made to the training guide, pages 20-22.
Requests for additional information
If additional information is required to make a determination on an authorization request, TurningPoint will reach out to the provider up to three times via a combination of phone and fax, within the designated turnaround timeframe for the case’s priority and plan type. You can find a copy of the request for information in TurningPoint’s provider portal.
Medicare intent to deny
Once an authorization request for a Medicare case has been denied, there isn’t an option available that could overturn the denial – appeal is the only avenue. Because of this, TurningPoint makes an Intent to Deny (ITD) call to the requesting provider ahead of a potential denial for Medicare cases.
During the ITD call, TurningPoint will help the provider take appropriate action to avoid an adverse decision by sharing:
- Rationale for the potential adverse determination
- Information about the option to schedule a peer-to-peer discussion before the final determination
- When the case is set to deny if additional information isn’t received, or a pre-denial peer-to-peer isn’t scheduled
Reconsideration requests
For commercial and Medicaid cases that have been denied – partially or fully – the provider may request a reconsideration before filing an appeal. Reconsiderations:
- Take additional information / documentation into account
- Return a decision within 5 calendar days
- May result in a revised determination without the need to proceed to an appeal.
A reconsideration can be a helpful step following a post-denial peer-to-peer review (P2P), though a P2P isn’t required to submit a reconsideration request. Note: Reconsiderations don’t always result in an approval.
Please see the updated TurningPoint Provider Training Guide (pages 19-22) for more details.
PHARMACY
Medicaid formulary changes coming Feb. 1, 2025
As decided by the Michigan Department of Health and Human Services (MDHHS), beginning Feb. 1, 2025, combination use of medications in the following Preferred Drug List (PDL) drug classes won’t be covered under the Medicaid Health Plan Common Formulary:
- Oral Hypoglycemic DPP4 (e.g., Januvia, Tradjenta), Oral Hypoglycemic-Combinations (e.g., Janumet, Jentadueto,)
- Incretin Mimetics (e.g., Byetta, Ozempic, Trulicity, Victoza)
- Anti-Obesity GLP-1s (Saxenda, Wegovy, Zepbound)
What do you need to do?
If you have impacted Medicaid patients, you’ll need to limit their therapy to a single drug from any of the above drug classes. If your patient continues treatment with two or more drugs from any of the above drug classes after February 1, their medication won’t be covered.
How are we communicating this change?
Impacted members and their prescribing providers will receive a letter in the mail detailing these changes and what steps they can take. Members are encouraged to contact their prescribing provider to discuss their treatment plan.
Why the change?
MDHHS works with health plans to create the Medicaid Health Plan Common Formulary - a list of drugs that all Medicaid health plans must cover. This formulary is reviewed quarterly by the Common Formulary Workgroup and the MDHHS fee-for-service (FFS) and Pharmacy and Therapeutics (P&T) Committee.
Questions?
Please review the coverage and criteria information found on our Medicaid formulary page. Pharmacy changes are posted quarterly in the Provider Manual, on our formulary updates page. Questions? Call us at 800.466.6642 . We’re available 8 a.m. to 7 p.m., Monday – Friday and from 8:30 a.m. to 12 p.m. on Saturday.
TRAINING OPPORTUNITIES
Register now for our January 30 billing & coding webinar
Join us for our first billing & coding webinar of 2025 to learn about:
- Navigating our Provider Manual & helpful resources
- Understand how your claim processed and why, right in prism
- Most common clinical edits we see applied to claims
- Asking a question about or disputing a clinical edit
- Submitting corrected claims
- 2025 telehealth billing updates
Can’t join us?
All webinars are recorded and posted to our website within a week of the event, so you can watch at your convenience.
REQUIREMENTS AND RESPONSIBILITIES
NCQA’s 2025 HEDIS audit is underway
Our Healthcare Effectiveness Data and Information Set (HEDIS®) team is contacting select providers by fax and phone to request medical records for the 2025 HEDIS audit. This is an annual audit conducted by the National Committee for Quality Assurance (NCQA) and used to measure quality of care across health care organizations in the United States.
The data you submit for this audit directly impacts how we invest in and enhance the benefits we offer our members. If you’re contacted, please submit all requested documentation by the deadline provided in your communication.
PLANS AND BENEFITS
Reminder: HMA members have access to Priority Health’s network
Priority Health launched a new product on Jan. 1, 2025, called HMA. HMA is a third-party administrator (TPA) product, but HMA plan members have access to Priority Health's PPO network.* Make sure your providers accept this health plan, the way they would with any Priority Health plan.
Providers should be on the lookout for this member ID card: 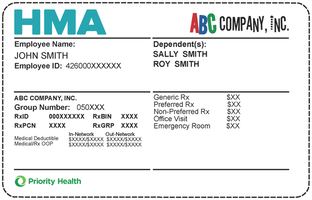
Providers should follow the instructions on the back of the card to submit claims, request prior authorizations, call customer support and more.
*Excluding Bronson Healthcare providers
Was there previous communication about the HMA product?
Yes, we communicated about HMA in 2024, including Priority Actions in November and December. We also communicated directly to providers via news items, prism communications and a provider webinar.
What resources are available for providers to work with HMA members?
Information and provider resources are all included or linked on our HMA provider landing page: priorityhealth.com/hma-providers. This page includes:
- Sample member ID card images
- Guidance on working with members: eligibility, prior authorization, claims, appeals, support
- Information on the HMA provider portal
- A breakdown of HMA tools and when to use them
- Information for providers outside of Michigan
- FAQs
- Additional resources, including a short video.
Members also have provider support cards to share with their providers, which include the reminder that HMA members have access to the Priority Health network and a link to the provider landing page.
Will HMA ever reach out to providers?
Yes, HMA may reach out directly if members report not being able to access in-network providers. After a provider sees an HMA member, HMA may also reach out for patient care needs, asking for medical records, etc.
Questions?
Reach out to your PSS consultant or call HMA’s support line at 833.865.0141.