ID.me identity verification now required for new prism users
Starting Apr. 25, 2024, any prism user registering for a new account will need to have their identity verified by ID.me.
Why are we making this change?
As part of our ongoing effort to ensure you and your patients’ data are as secure as possible, we’re implementing additional identity verification for new users who register for prism through ID.me.
Who’s impacted?
Only users registering for a prism account for the first time will be impacted. Those who already have prism access will not be impacted. Anyone reactivating their prism account after 120 days of inactivity won’t be required to use ID.me for identity verification.
How will this affect the prism registration process?
When registering for prism, you’ll be prompted to verify your identity with ID.me by creating a new account or logging into your existing ID.me account before you’ll be able to finish prism registration. Use this ID.me account creation guide for step-by-step details and helpful screenshots.
Verification can take 2–10 minutes depending on if you already have an ID.me account or not. ID.me is used by many other government agencies and businesses, such as the IRS, so you may already have an ID.me account.
After verification, you’ll be redirected back to prism to continue adding your provider demographic information. Once submitted, account approval may take up to 48 hours, with additional time for provider affiliation approval from your group’s prism Security Administrator (pSA).
Will ID.me keep provider information safe?
Yes. ID.me meets the federal government's most rigorous technical and policy controls for privacy and information security. It encrypts all personal data and is used by hundreds of organizations, including government agencies and commercial organizations, to keep people's personal information safe.
Why does ID.me need my Social Security number?
ID.me’s verification process requires collecting sensitive pieces of information, like your Social Security number. ID.me needs this information to uniquely identify you, a critical step to prevent impersonation and fraud and to protect your practice’s and your patients’ data.
When you provide your Social Security number as part of ID.me’s identity verification process, that information is not shared with Priority Health.
Do users who live outside the United States need to do anything differently?
Yes. When you reach the “Verify your identity” step of the process, tap the hyperlinked text at the bottom that says, “I don’t live in the United States.” Then follow the on-screen prompts. You’ll be required to provide identification documentation and participate in a video call with a Trusted Referee from ID.me for full verification. See this video demo for guidance.
If I already have an ID.me account, should I create a new one when registering for prism?
No. Only create an ID.me account if you never created an account in the past. Simply sign in to your existing account and follow the prompts. If you need a specific email associated with your ID.me account, sign in to your account and add the new email address.
If you already have an ID.me account and can’t sign in, you will need to recover access to your account. For sign-in troubleshooting tips, visit ID.me's help page.
More questions?
Check out our FAQ resource for answers.
Providers may need to resubmit incorrectly denied COVID vaccine claims for payment
Between August 2023 and February 2024, some COVID vaccine claims were denying when they shouldn’t.
Our teams identified and resolved the root cause of the issue, automatically reprocessing for payment. However, some providers have identified claims that weren’t reprocessed.
Identifying impacted claims
Impacted claims include those for CPT codes 90480 and 91318-91322 with denial codes Q01 or Q02 (Not Contracted) or clinical edit y28 (Invalid HCPCS procedure).
How to get paid
If you’ve identified any applicable claims that weren’t reprocessed, please follow the instructions in our Provider Manual for resubmitting claims.
We value your partnership and the care you provide our members, and we sincerely apologize for any inconvenience this has caused. Thank you for your patience and understanding.
Hearing aid providers: Invoice submission for Medicaid members is no longer necessary
We’re always looking for ways to make working with us easier for our providers. That’s why we’re happy to share that, effective immediately, hearing aid providers no longer need to send us an invoice for a Medicaid member’s hearing support device.
We’re now able to accept the device’s model information on claims. It’s a small change that will hopefully save these providers valuable time and energy.
What providers need to do
Providers should review the MDHHS Hearing Aid Contract Models document for device naming and model number conventions, and enter the following on their claims:
Model number (exact match) Manufacturer name Model name (as many characters as allowed in the field)
For example: 211921xx Beltone AMAZE 6 66
- Electronic claims (preferred): On the 837 claim form, enter the italicized information for the billed device into Box 19, Export Loop = 2300 (NTE;PWK)
- Paper claims: On the standard CMS-1500 claim form (02-12 version or later), enter the italicized information for the billed device into Box 19.
More information
Additional information is available to providers on the following Provider Manual pages:
PriceMyMeds launching on April 25 to increase prescription drug affordability
Beginning Apr. 25, 2024, we’re offering a new pharmacy program called PriceMyMeds to our commercial (group and individual) members. PriceMyMeds helps members save on prescription medications by automatically finding the best price for a prescription at nearby in-network pharmacies.
This new benefit is a key part of our ongoing goal to better support our members in getting the care they need by making sure prescription drug costs are not a barrier to the care you provide.
How does PriceMyMeds work?
When a member’s prescription is filled at a pharmacy, PriceMyMeds automatically searches for and applies savings opportunities, when applicable. Members will also have access to the PriceMyMeds app, allowing them to sign up to receive alerts when greater savings opportunities are available at other pharmacies in the area. When members use the PriceMyMeds app to locate a better price at an alternative pharmacy, PriceMyMeds will provide instructions on how to 1) ask for a price match or 2) work with their pharmacist to complete a prescription transfer.
Check out our Provider Manual for more details.
How is PriceMyMeds different from Price Assure?
Price Assure automatically incorporates discounts through GoodRx into drug pricing and applies it at the point of sale without anything being required of members. PriceMyMeds searches for all freely available discounts. A key difference is that Price Assure only applies to a small set of drugs. With PriceMyMeds, members can access savings through other discounts on a wide variety of drugs.
Members will be given the lowest possible price through either PriceMyMeds or Price Assure without any action needed on their part.
How is PriceMyMeds different from SaveOnSP?
SaveOnSP is only for select specialty medications and focuses on manufacturer assistance. PriceMyMeds finds freely available discounts on retail prescription drugs, without relying on manufacturer assistance.
Are any medications excluded from PriceMyMeds?
There are a few categories of drugs that are excluded from PriceMyMeds:
- Any drug eligible for the SaveOnSP program, for eligible members
- Non-formulary drugs
- Certain brand drugs
- All opioid drugs
- Drugs available at $0 cost-share through the Affordable Care Act
- Drugs available through a Priority Health commercial rider
- Drugs available through a Priority Health commercial rider
How will members be notified about PriceMyMeds?
Members will receive an email or mailed notification with information about how to activate a free account and download the app. Once the app is downloaded, members can load medication lists into the app and immediately begin searching for discounts at all local in-network pharmacies.
How will this affect providers?
Occasionally, you’ll need to send the prescription to a new pharmacy if the member’s current pharmacy doesn’t accommodate transfers.
The main benefit is patients having better access to affordable medications, which is a win for everyone.
Formulary changes for commercial group and individual members coming July 1
In January and July of each year, the Priority Health Pharmacy and Therapeutics committee make changes to the commercial group and individual formularies to ensure our members have access to safe, effective and affordable drugs.
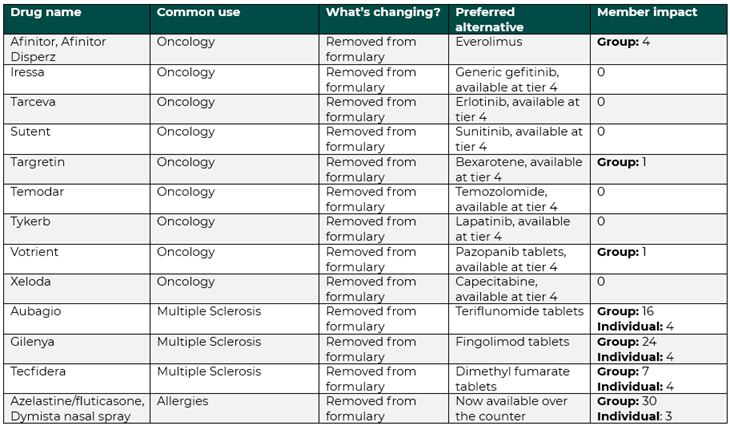
Commercial and individual formulary changes take effect on July 1, 2024
Beginning July 1, 2024, 13 drugs will be removed from our commercial group formulary and 1 drug will be added to our site-of-service policy. These changes will impact 95 of our commercial group and individual members.
Commercial group and individual formulary changes
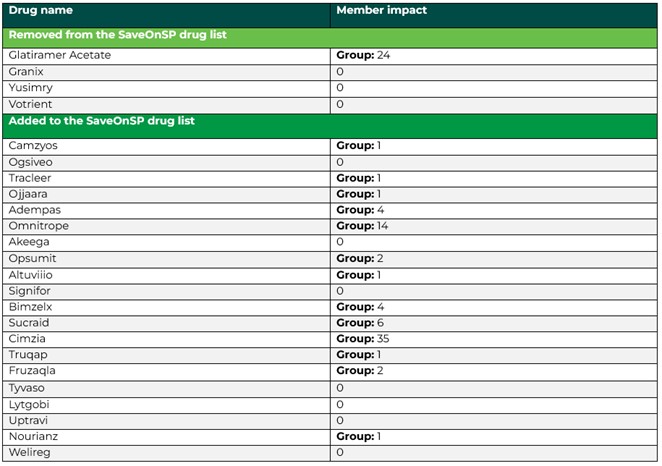
SaveOnSP program changes
24 drug changes will go into effect that will either remove or add a specialty drug at the $0 out of pocket cost through the SaveOnSP program. These changes will impact 103 members.
If the removed drugs from the SaveOnSP list are included in the formulary, the drugs will no longer be eligible for the $0 out of pocket cost but may be covered through the members’ cost share plan. No alternatives will be offered for removed drugs.
Members are encouraged to contact the SaveOnSP team with questions. The complete SaveOnSP drug list is available as an attachment on the Approved Drug List.
SaveOnSP drug list changes
Aligning with Cognizant engine changes as they’re released
Beginning with the 2024 performance year, we’ll update our system to use Cognizant’s new data engine for HEDIS and PIP when it’s released annually in late summer / early fall, rather than waiting until after settlement as we have in the past.
This change:
Follows industry standards
Improves the alignment of our HEDIS and PIP rates and resources.
Will have minimal impact for the 2024 performance year
Background
Cognizant, our vendor for measuring performance on HEDIS gap closure, updates their data engine annually, releasing the updated version in the late summer / early fall. Until now, we’ve continued to use the previous year’s engine for the current program year through settlement.
Starting with the 2024 performance year, we’ll switch to the new engine when it becomes available – likely in August or September. We’ll continue to follow Cognizant’s scheduled engine changes moving forward.
What’s the anticipated impact to you?
- Filemart reporting will reflect 2023 HEDIS measure specifications until Cognizant releases the new engine. At that time, Filemart reporting will begin to reflect 2024 HEDIS specifications.
- 2024 PIP will be settled with 2024 HEDIS specifications, which are provided in the 2024 HEDIS Provider Reference Guide and referenced in the 2024 PIP Manual. Access both online (login required).
- The differences in measures between 2023 and 2024 are minimal. The only impacted measure is HbA1c (see below for details).
HbA1c updates from 2023 to 2024
The 2023 HEDIS Hemoglobin A1c Control for Patients with Diabetes (HBD) measure will be updated in 2024 and renamed to be the new Glycemic Status Assessment for Patients with Diabetes (GSD) measure.
The following are the differences providers will see with this update:
#1. Identifying diabetics
Members qualify as diabetics by medical or pharmacy claims. Requirements for both have changed.
- Pharmacy claims: In addition to having a diabetic medication dispensed, the GSD measure adds a requirement for diabetes diagnosis this year or last year on any claim except a lab. This makes the pharmacy option more restrictive.
- Medical claims: The GSD measure simplifies but broadens the diabetes diagnosis claim requirements.
- HBD: Different requirements based on claim type (i.e., one claim for acute inpatient or two claims for outpatient visits)
- GSD: Two claims, any type but lab
#2. Exclusions
- Removed exclusions: GSD removes the required gestational diabetes, steroid-induced diabetes and ovarian syndrome exclusions.
- Changes exclusions: GSD changed the optional exclusion definitions a little
- Frailty: Adds a “no lab claims” requirement
- Advance illness: Removes the place of service (POS) restrictions (i.e., claims-based diabetic identification above) and adds a “no lab claims” requirement
#3. Numerator qualification
- Added LOINC code: GSD adds a new LOINC code for A1c test: 97506-0 “Glucose management indicator”.
- New CPT modifier exclusions: GSD adds the following CPT modifier exclusions to CPT II codes. Of these modifiers, we only saw 8P in 2023 used on 237 claim lines.
- 1P – Performance Measure Exclusion Modifier due to Medical Reasons
- 2P – Performance Measure Exclusion Modifier due to Medical Reasons
- 3P – Performance Measure Exclusion due to System Reasons
- 8P – Performance measure reporting modifier-action not performed, reason not otherwise specified
Helping you get 2024 medication adherence reports into the right hands
As you know, our medication adherence reports include time-sensitive, actionable information that helps you close care gaps for your patients and increase your PCP Incentive Program (PIP) earnings. As we approach the release of our first monthly medication adherence reports for 2024, we’d like to offer you the opportunity to provide additional contacts that you’d like us to send the reports to.
If you’d like us to CC additional stakeholders in your organization when sending your monthly medication adherence reports, please email the following information to your Provider Strategy & Solutions Consultant:
- Contact name(s)
- Contact email(s)
- Role(s)
Stakeholders can include care managers, embedded pharmacists or anyone using the reports for direct patient care.
What are medication adherence reports?
These reports focus on your Medicare patients who use their Priority Health drug plan benefit to fill medications for diabetes, hypertension or cholesterol. They highlight which patients are compliant with their medications, and which are noncompliant or at risk of becoming noncompliant.
What’s included in the reports?
Each report includes the following:
Member information
- Patient name
- Patient date of birth
- Patient’s Priority Health plan benefit package
Medication information
- Medication name
- Medication day supply
- Medication refill due date
- Date to non-adherence: The date your patient is no longer compliant with taking their prescribed medication
Tips for interpretating the medication adherence report
- Help tab: Helps you navigate the report
- Priority Report tab: Lists members who are non-compliant or at risk of becoming non-compliant with their medication
- Full Adherence Report tab: Lists members who are compliant with their medication