Requirements and Responsibilities
2023 PriorityMedicare D-SNP Model of Care training is due Dec. 31
Who needs to complete training?
All providers who are part of the Priority Health Medicare Advantage network need to complete training. This includes specialists, ancillary providers, or anyone part of an ICT (interdisciplinary care team) for a D-SNP member. This is a CMS requirement.
How do providers complete the training?
Providers can complete our training using one of two options.
Option #1: Bulk attestations
You can group our D-SNP MOC training with existing, required training (like compliance training) so you can submit attestation for providers at the same time. If this option is selected, you’ll need to:
- Distribute training to your providers using this link.
- To attest to training, you must fill out the roster template with providers who’ve received training. If you choose to submit a provider roster, only the Priority Health MOC roster Excel sheet provided will be accepted.
- Send attestation rosters to DSNPtraining@priorityhealth.com.
Option #2: Virtual training (only takes 15 minutes)
Training is available as an on-demand webinar and only takes 15 minutes for providers to complete. Online training can be accessed here. Provider registration for the on-demand webinar counts as attestation, which means no additional documentation is required.
Be sure to submit the correct provider NPI
Ensure the correct provider NPI number is included when submitting the provider roster or registering for the online training. If the NPI is incorrect, the provider’s status will be marked "incomplete" in our system. To correct an "incomplete" status due to an incorrect NPI, resubmit the provider roster or re-register for the online training with the correct provider NPI.
Your Provider Strategy & Solutions consultant will send you a report with providers who still need to complete training.
An important update regarding transplant services and CAR T-cell and gene therapies
Effective Mar. 1, 2024, all bone marrow transplants, organ transplants and CAR T-cell and gene therapy for Priority Health commercial members will be managed through the Emerging Therapy Solutions (ETS) network. This change doesn't include Medicare and Medicaid.
To ensure a seamless transition, ACNs that provide transplant services and CAR T-cell and gene therapies are encouraged to finalize an agreement with ETS before Mar. 1, 2024.
Why are we making this change?
Priority Health is a nonprofit health plan with low administrative costs that spends nearly 90 cents of every dollar on our members. Transplants, CAR T-cell, and gene therapies are specialized and constantly changing. That's why we're partnering with an industry leader—ETS—to ensure our members get the care they need.
Who is ETS?
ETS’s mission is to help its patients across the nation get the treatment they need for rare and complex conditions through bone marrow transplants, organ transplants, and cell and gene therapies.
Is the prior authorization process changing for transplants or CAR T-cell or gene therapy?
No. For transplants, please continue to fill out the appropriate prior authorization form (available for download on our provider manual) and either attach it to your submission in the GuidingCare portal or submit it via fax, to the number indicated on the form. CAR T-cell and gene therapy prior authorization requests should continue to be submitted via the Surescripts portal.
You’ll continue to work with Priority Health directly for claims and billing.
What are the next steps for ACNs that provide transplant services and CAR T-cell and gene therapies?
If you don’t already have a contract with ETS, they have reached out to your organization.
What happens if you don’t have a contract with ETS by Mar. 1, 2024?
For providers not contracted with ETS by Mar. 1, 2024, ETS will perform Single Case Agreement (SCA) negotiations for services rendered by a non-contracted facility or provider. SCAs will not affect member benefits or the amount the member is responsible for.
Where can I reach ETS if I have questions, or if I need to secure a participation agreement?
- Toll Free: 877.445.4822
- info@emergingtherapies.com
Incentive Programs
2023 PIP Q4 focus measure pre-payments
The fourth and final quarterly chronic disease focus measure pre-payments for the 2023 PCP Incentive Program (PIP) were issued on Dec. 15.
If your ACN is set up with us to receive electronic funds transfer (EFT), your pre-payment will be processed as soon as your bank accepts the file. If not, your pre-payment will process by paper check to your ACN remittance address on file.
Get more information
For more information on focus measures, pre-payment and settlement, see our 2023 PIP manual (login required).
Questions?
Contact your Provider Strategy & Solutions consultant.
2023 PIP supplemental data audits will take place in January 2024
Our 2023 PCP Incentive Program (PIP) supplemental data audits will begin in early Jan. 2024. This audit process helps us to ensure the integrity of our data and the accuracy of your PIP settlement payout.
Audit notification & timeline
On or around January 10, you’ll receive a secure email with a list of requested medical records. You must return the audited medical records within two weeks of the notification. Failure to do so will result in a 50% penalty on your 2024 PIP payout.
How audited records are selected
Records selected for audit are based on any non-standard supplemental data (Patient Profile and Report #70) provided from Jan. 1 – Dec. 31 of the program year. The records are randomly selected based on the ACNs membership as follows:
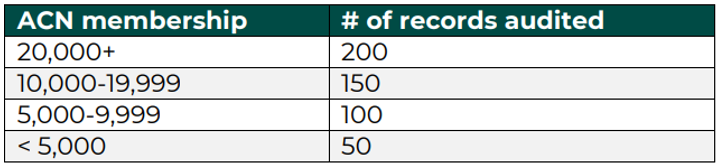
If there are fewer records than the maximum allowed, all records will be subject to audit.
More information
Learn more about the audit process in our 2023 PIP manual (login required, see Appendix 2: Supplemental Data).
Billing and Payment
Professional providers: Use POS 02 and 10 for virtual services starting Jan. 1
To align with changes made by the Center for Medicare and Medicaid Services (CMS), we’re updating our virtual care billing guidelines for professional providers. Beginning Jan. 1, 2024, professional providers will use the following place of service (POS) codes for virtual care services for our commercial members, along with the appropriate modifier:
- 02: Telehealth provided other than in patient’s home
- 10: Telehealth provided in the patient’s home
This update is a shift back to pre-COVID-19 public health emergency billing guidelines for POS. There will be a grace period, until Feb. 1, 2024, to allow providers to update their billing practices.
Virtual care billing guidelines for facilities – which align with CMS for reporting of revenue codes, HCPCS and modifier use – won’t change. For more information on virtual care billing, including billing guidelines for Medicare and Medicaid, see our provider manual.
Replacing APCD extracts with improved, data-rich file in the coming months
As we continually strive to provide you accurate, easy-to-use data, we’ll be phasing out our All Payer Claims Data (APCD) extracts in 2024 – transitioning to a more robust, data-rich file that includes the member and claims data you need.
This transition will take place over the course of several months, during which you’ll have the opportunity to test and update your systems to ingest the new file while still receiving the APCD extracts.
Testing our new data dictionary
We’ve made available a data dictionary/file layout to compare what you receive today through APCD with what we’re preparing for the updated files. This Excel spreadsheet lists the fields appearing in each extract with a data description, type, size and format.
SFTP setup
While APCD files are shared via Filemart, the updated files will be delivered to ACNs by Secure File Transfer Protocol (SFTP). As more of our reports and data move to SFTP (including our new Disease Burden Management program), we encourage you to get set up with us if you haven’t already.
Questions, feedback and next steps
In the coming weeks, we’ll connect with you on rollout timing and needs, including a test file tailored to your ACN as well as additional training and materials to support you through this transition.
If you have questions or feedback, or need support getting set up with SFTP, contact your Provider Strategy & Solutions consultant.
Thank you in advance for your support and partnership.
Training Opportunities
Register now for our 2024 Virtual Office Advisory (VOA) webinars
Our virtual office advisory (VOA) webinars continue to be a key way of connecting with you and your staff about important updates and reminders.
We’re excited to have connected with more of you than ever before this past year. In 2023, we saw a 39% increase in average attendance from 2022.
That’s a clear sign to us that the information we’re providing through our VOAs is important to you. So let’s keep it going in 2024.
- Feb. 8, 2024: general audience
- Apr. 11, 2024: billers and coders
- June 13, 2024: general audience
Click the links above to register for each respective webinar. No need to wait — registration is already open. Specific topics will be announced a month prior to each VOA.
Where can I find registration links and recordings of past VOAs all in one convenient place?
All this can be found on the VOA page in our provider manual.
Stay tuned for more news, as we continue working to bring you content that’s relevant to you when it’s most convenient to you.
myStrength program will be renamed to Teladoc Health Mental Health on Jan. 1, 2024
Effective Jan. 1, 2024, the myStrength program will be renamed Teladoc Health Mental Health and migrate to Teladoc Heath’s app. The myStrength digital courses and member information will be available on the Teladoc Health platform, plus enhanced features – coming soon. More details about the enhanced features will be in early 2024.
The program guide will temporarily be unavailable but will return in 2024 with additional features.
What do members need to know?
Beginning Jan. 3, 2024, Teladoc Health will contact all members with a myStrength account via email to inform them of changes to the platform and instructions on how to transfer their account information.
Members interested in creating a new account should follow the instructions below.
- Visit priorityhealth.com/mentalhealth and click sign up.
- Provide personal information to create the account.
- Check the ‘I have a code from my employer, insurance or Teladoc Health’ box and insert the access code PHMH.
- Answer additional questions to complete the sign up process.
Help and support
Members can reach out to Teladoc Health’s member support team for assistance by calling 800.835.2362 or emailing membersupport@teladochealth.com.